$400.00 Original price was: $400.00.$350.00Current price is: $350.00.
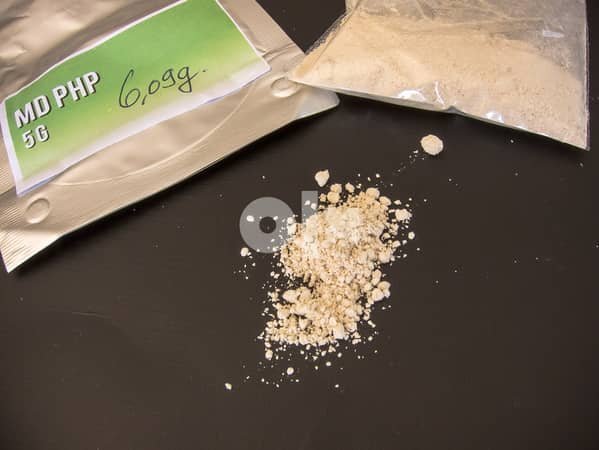
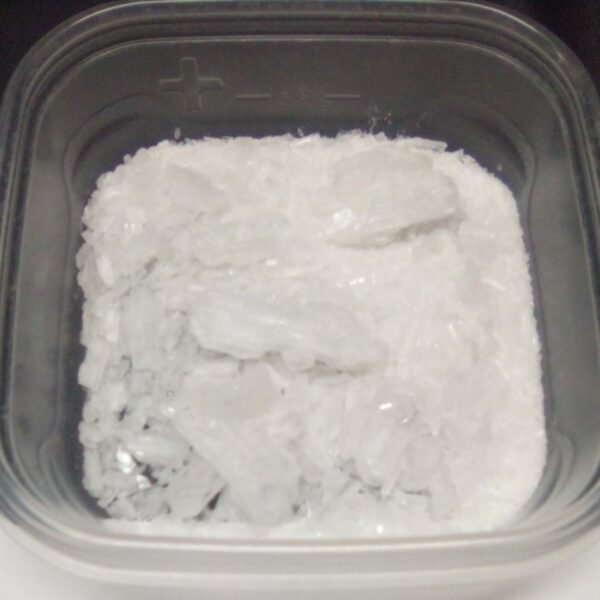
Generic name: Ketamine
Brand name: Ketalar
Dosage form: Injection 200 mg/20 mL (10 mg/mL), 500 mg/10 mL (50 mg/mL), and 500 mg/5 mL (100 mg/mL)
Drug class: General anesthetics
Ketamine, chemically known as (RS)-2-(2-chlorophenyl)-2-(methylamino)cyclohexanone, is a synthetic compound classified as a dissociative anesthetic. Originally developed in the 1960s for use in human and veterinary medicine, its primary function has historically been as an anesthetic agent. The chemical structure of ketamine features a cyclohexanone core with an aromatic ring, allowing it to target the N-methyl-D-aspartate (NMDA) receptor in the brain, leading to its anesthetic and analgesic properties.
Ketamine is primarily administered intravenously or intramuscularly, demonstrating rapid onset of action and a short duration of effects. In surgical settings, it is utilized for its ability to induce dissociation, a trance-like state where the patient is not fully conscious yet remains pain-free. Its unique properties make it especially beneficial for trauma patients and in emergency rooms, where traditional anesthetics may be less effective.
Importantly, ketamine has been approved for several medical purposes beyond anesthesia, including management of acute pain, sedation during procedures, and as a rapid-acting treatment for depression, particularly in patients resistant to conventional antidepressants. However, ketamine’s classification as a drug also extends to its recreational use, where it is taken for its hallucinogenic effects, often in social or party settings. This non-medical use can lead to various health risks and potential addiction, inciting concerns among healthcare providers.
Understanding the context of ketamine as both a therapeutic and recreational substance is essential to comprehend its dual nature, revealing both the potential benefits in medical applications and the dangers associated with misuse. As research continues to evolve, ketamine’s role in contemporary medicine remains a critical area of exploration.
Ketamine, a dissociative anesthetic, has been utilized in medical procedures since its FDA approval in 1970. It is particularly valued for its unique ability to induce anesthesia while maintaining hemodynamic stability. This characteristic makes it especially beneficial in emergency situations where rapid anesthesia is required. Unlike other anesthetic agents, ketamine causes analgesia and sedation without necessarily impairing respiratory function, ensuring that patients can be managed safely even in less controlled environments.
When administered, ketamine primarily exerts its effects through NMDA receptor antagonism, disrupting the transmission of pain signals in the central nervous system. This mechanism not only allows for effective anesthesia during surgical procedures but also plays a vital role in pain management post-operatively. The duration of action and the fast onset time are critical advantages for clinicians striving to provide immediate relief during and after surgery.
Dosage and administration methods for ketamine can vary based on patient needs and the nature of the procedure being performed. It can be delivered intravenously, intramuscularly, or as a nasal spray. For surgical use, the standard dosage typically ranges from 1 to 4.5 mg/kg when administered intravenously. Considering its potent anesthetic properties, it’s essential for healthcare providers to tailor dosages to individual patient profiles, taking into account factors such as age, weight, and overall health status.
Despite its advantages, the use of ketamine as an anesthetic is not without potential side effects. Some patients may experience hallucinations, increased blood pressure, or dissociation during recovery. Therefore, monitoring and post-operative support are crucial following its administration. This careful approach ensures that the benefits of ketamine’s anesthetic properties are leveraged while minimizing adverse effects, thus reinforcing its role in modern anesthetic practice.
In recent years, ketamine has emerged as a promising alternative for the treatment of depression, particularly in cases where traditional antidepressants have proven ineffective. Originally used as an anesthetic, ketamine’s ability to rapidly alleviate depressive symptoms has garnered significant attention, leading to a growing body of research and clinical trials. These studies suggest that ketamine acts on the brain’s glutamate system, offering a unique mechanism of action that differs from that of conventional antidepressants, which primarily target serotonin and norepinephrine receptors.
Unlike traditional antidepressants, which often take weeks to exhibit therapeutic effects, ketamine has been shown to produce rapid improvements in mood, sometimes within hours of administration. This rapid response is particularly beneficial for patients experiencing severe depressive episodes or suicidal ideation. Current research indicates that ketamine may induce synaptogenesis, the formation of new synapses, thereby contributing to its quick antidepressant effects. This distinct pharmacological profile sets ketamine apart and positions it as a viable treatment option for major depressive disorder and treatment-resistant depression.
Despite its potential, the off-label use of ketamine raises several considerations regarding safety and efficacy. The long-term effects of repeated ketamine treatments are still under investigation, with some studies indicating possible risks, including dissociative symptoms and addiction concerns. Clinicians must weigh the potential benefits against these risks, particularly as ketamine therapy is not yet FDA-approved for depression treatment. Ongoing clinical trials are likely to shed light on the safety, dosing, and optimal administration methods, as well as the neurobiological mechanisms underlying its therapeutic effects. As evidence accumulates, ketamine’s role in mental health treatment continues to evolve, reflecting a paradigm shift in how we approach depression management.
Ketamine, originally developed as an anesthetic, possesses hallucinogenic properties that have led to its recreational use in various social settings. This misuse is often associated with a desire for altered states of consciousness and a dissociative experience. Users typically seek the euphoric and surreal sensations that can occur under the influence of the drug. However, the allure of these effects is accompanied by significant risks, including the potential for addiction, harmful psychological impacts, and adverse physical reactions.
Illicit use of ketamine commonly occurs in nightclubs and parties, where individuals may administer the substance in various forms, such as snorting or injecting. The lack of regulation and quality control in illegal contexts further exacerbates the risks associated with ketamine abuse. Users may find themselves in unpredictable situations, as the drug can lead to disorientation, impaired motor skills, and reduced sensory perception. The effects often vary between individuals, which can make the experience perilous and unpredictable.
One of the most alarming risks of ketamine abuse is its reputation as a “date rape” drug. Its capacity to induce profound dissociative states and short-term memory loss raises concerns regarding its potential to facilitate sexual assault. Victims may find themselves unable to recall events that occurred while under the influence of ketamine, rendering them vulnerable to exploitation. This aspect highlights the critical need for increased awareness and education surrounding the potential dangers of ketamine misuse.
Moreover, repeated use of ketamine can lead to psychological dependence, where individuals feel compelled to continue using the drug to achieve desired effects. This can result in a cycle of abuse that may harm mental health and overall well-being. Understanding the dark side of ketamine is crucial for fostering a safe environment and preventing its detrimental impact on individuals and communities.
In recent years, ketamine has emerged as a multifaceted compound, demonstrating a unique duality in its applications within the medical field. Originally developed as a dissociative anesthetic for surgical procedures, ketamine has gained recognition for its potential to treat various mental health conditions, including depression and anxiety disorders, showcasing therapeutic benefits that could revolutionize treatment paradigms. However, while the clinical advantages of ketamine are notable, it is crucial to approach its use with a balanced perspective, considering both its efficacy and the risks associated with its misuse and abuse.
The growing interest in ketamine’s role as a treatment option necessitates thorough research to fully understand its pharmacological effects and long-term impacts on different populations. Current studies have highlighted its rapid antidepressant properties, which can provide significant relief for individuals who have not responded to traditional therapies. This potential could signify a paradigm shift, especially in treating resistant mental health disorders. However, the appeal of its rapid effects also presents a risk of illicit use, prompting concerns regarding addiction and dependence. Thus, healthcare professionals must remain vigilant in distinguishing between therapeutic applications and recreational misuse.
To support the future integration of ketamine into clinical practice, ongoing research and regulations will be essential in establishing guidelines for its responsible use. The medical community is called upon to facilitate a deeper understanding of the substance to mitigate associated risks while capitalizing on its significant therapeutic potential. By advocating for informed and judicious prescribing practices, as well as promoting awareness of the dangers of abuse, stakeholders can contribute to a balanced approach that prioritizes patient safety without stifling innovation in treatment options.